Having cancer is like no other experience. The strangeness of it. Although it’s a common disease does anyone expect to get it? I had thought maybe I would get breast cancer which my sister has had twice. But I’ve got colon cancer. Very unexpected. I’ve been keen on health foods for 50 years. I think I understood “reduced risk” as “no risk.” It was a shock.
Because I have IBS my cancer symptoms were masked by my IBS symptoms. The symptoms got worse when covid happened. I was very frightened and stressed by covid. I remember saying to my partner – I’m more frightened of catching covid than cancer. So I delayed going to the doctor for six months. I started to use a FODMAP diet, which reduced my symptoms a lot, so I was reassured. Then I had a tiny bit of blood. I thought it was from an internal haemorrhoid, which I’d had before. I went to the doctor. The blood test I had must have shown high cancer markers, but no one told me.
I was sent for a colonoscopy, which is an internal scan of the colon. I didn’t have sedation, and I saw the tumour, but I still thought maybe it’s something else. It was white and round.
After the procedure I was wheeled out to the tiny curtained space where I had been waiting before. I was lying on the hospital trolly bed. Three men crowded into the space, standing looking down at me. One of them spoke to me at length. All I heard was “we found a tumour”. I’ve since thought this was not well-managed. I needed one person, sitting down, explaining simply what they had found.
I was in shock. I could feel myself being turned into “a patient” by how the doctor spoke to me.
I had a scan which showed that cancer had spread into my lungs. The surgeon explained that this cancer was inoperable. Unfortunately he explained this rather ineptly and I wasn’t sure what he was saying. Eventually I said to him “Are you saying I’m going to die from this?” and he replied “Yes”. I was with my partner. We were both in shock. So I almost didn’t feel anything. We were taken to the specialist nurses room. He was very nice but I only remember him talking to us about claiming benefits. His timing was off. I said no, we don’t need to. ( But months later, I did claim Attendance allowance.)
A month later I had an operation to remove the colon tumour, which was likely to block my bowel if not removed. This was a stroke of luck for me. Many people with a similar diagnosis had their operations postponed because of the Covid crisis, but mine would have become an emergency situation if not dealt with.
I was very frightened about having the operation. I thought I might die. But all went well and I didn’t have to have a stoma bag. I count myself very lucky that I avoided having one.
Because of Covid I was in a private hospital that had been rented by the NHS. This meant I had a private room with ensuite bathroom. Luxurious, no- one’s snoring to tolerate!
After the operation the staff of the hospital commented on how quickly I was recovering, both surgeons and nurses. I put this down to having adopted an anti-cancer diet which I had been on for a month, almost since my diagnosis. I had been depressed immediately after my diagnosis, but after three weeks I discovered the idea of anti-cancer diets, devised one for myself, and the depression went. I took my own food into the hospital, and family members dropped off supplies at reception. The hospital had given me a “ protein drink” that I was to take pre- and post surgery. I looked at the ingredient- list, in case it might trigger my IBS- it was made of water, sugar and a few vitamins. This was supposed to make me recover more quickly from the operation. ( Probably because people often lose their appetite in this situation, and this was calories. ) I replaced it with a mixture of grape juice, pineapple juice and water, which would give me the same amount of calories and some vitamins. When challenged, I just told hospital staff what was in the “ protein “ drink.
The diet I had adopted was vegan and organic, with lots of carrot juice and supplements, and mostly raw food. I think it really helped me. I had plenty of energy.
I was reluctant to have chemotherapy. My sister had had a terrible time having chemotherapy. After three months I had a scan which showed my cancer had not grown and was stable. This encouraged me to continue with the diet and not have chemotherapy. But after another three months I started to get a severe pain in my lower back. I was reluctant to have a scan, because of the radiation involved, but eventually I did.
This was in the summer, and we had left London to be at the coast for several months. This meant I did not have my alternative treatments. I had been having cranial osteopathy. I don’t know if not having that allowed my cancer to start to grow again. It’s impossible to know. Scans showed that I have several tumours in various places around my body. At this point I decided to have chemotherapy, as the pain I was experiencing was caused by a tumour pressing on my sacrum.
The effect of the pain was to completely take away my appetite. It also made all food and drink, even water, taste horrible. I lost weight. I was given morphine to control the pain.
Luckily the chemotherapy has been fine, although some people had told me it would be terrible, which wasn’t helpful. I have had a few side-effects but nothing too difficult, and within a few weeks my back pain had gone.
I have now had six months of chemotherapy at three-weekly intervals. A recent scan has shown that my tumours have shrunk by 30%.
One of the difficulties of this situation for me and I’m sure for others, is trying to grasp the reality of death. In fact a large part of me does not believe I am going to die soon. I don’t feel near death, and other people don’t experience me as near death.
The first oncologist I saw told me that the survival rate for my situation, without chemotherapy, was three months from diagnosis. I was already 31/2 months from diagnosis at this point. She also said that with chemotherapy my prognosis would be 1 to 2 years. She told me that chemotherapy would be awful, and asked me if I wanted a leaflet about this, which I did. Then she laughed and said “this will put you off even more.” I found her so unempathic that I decided to change to a different oncologist. Luckily I find the new one much easier to get on with.
I am now about 18 months from diagnosis and my health remains good. I get tired, but not so much that I can’t lead a normal life. I grow food in my allotment, I work a few hours a week as a psychotherapist , I see friends and family.
I have had good support from the cancer psychology department at Homerton Hospital.St Joseph’s hospice is also a great source of support.
I can see I’m veering away from the subject of death again. When I used to see the psychologist I used to do that. ( He left, and I’m waiting for a replacement.)
At first I was very frightened of how I would die. My mother died when I was very young, of a lung disease. She took about 3 years to die, coughing and hawking up denatured blood and pus and lung tissue. Both oncologists reassured me that this would not happen to me, rather I would become more tired, sleep more, a “ gradual fade”. This has been confirmed by friends whose family members have gone through that process. I only half believe it though.
July 2022
Now I’m on my allotment picking gooseberries trying to think about death. My mind veers off constantly to gooseberry crumble or a friend who is on the journey here to meet me. Thinking about death inevitably makes me think about what it is going to be like when it happens. Doctors have told me lots of different things but one consistent thing is they would expect me to have another six months of life. They told me this ages ago but also that it would be peaceful and I would become more tired, gradually fading away. I was worried about haemorrhages and pain. I hope they’re right. Two different doctors separately told me this, so I suppose it’s probably what they think will happen. I don’t know what actually stops you living in that situation. Something grows and stops something working I suppose. I really don’t know enough about the body. It still doesn’t feel real even saying it now. I don’t feel that it’s going to happen, because I don’t have any signs of it happening. A week or two ago I was terribly tired after overworking because I’d got behind with something. Much tireder than I would normally get. That worried me.
I took some homeopathy which helped a lot. I speak to a homeopath regularly, and the great thing about that is she can help me with things the doctor can’t help me with, like feeling so tired.
I’ve been very lucky in that I’ve had quite a lot of counselling from the Homerton psychology team. I’ve had several different people because one went on maternity leave and then the replacement I didn’t like. Then I had a nice one, but he was filling in for the maternity leave, and now he’s left because he got a permanent job. It was very upsetting each time I had to say goodbye to a therapist unexpectedly.
What is very useful to me about the therapy is that that I don’t have to worry about how they feel. I don’t have to think whether they are going to be really shocked and upset because I’m talking about cancer. This concern stopped me telling other people for quite a long time. Apart from my children, who are adults, I didn’t tell anybody except the closest of friends, and one of my sisters, for months, because I didn’t want to upset them.
I felt very much that I could talk to M, the therapist, about anything. If I had a difficulty talking about something, it was very much my difficulty, not to do with him. I could cry, which I was finding difficult with family and friends, I could be angry at my situation, I didn’t have to hold back. He helped me enormously, and it was very hard for me when we had to part.
I had a letter from the Homerton saying I was discharged from the service. This was such a shock that I literally didn’t take it in, didn’t remember M saying this would happen. I’d had approximately a year of therapy with them, so I suppose that’s the limit. It was two months later that my partner came across the letter and we talked about it and I realised that I had come to the end of therapy with that service. I felt very sad and somewhat angry. I had so much not allowed myself to know this.
Now I’m contemplating whether to ask them for more, ( unlikely to be successful, I think), or move on to other services that offer specialist counselling and therapy.
I ll probably apply to St Joseph’s Hospice, where I’ve had some physical therapy, to access their counselling service. I need to talk to someone neutral, outside the family and my group of friends, who can give me support and listen without my feeling I must look after them. That’s a big block for me, but luckily I don’t feel it when talking to a therapist.
I have a strong urge to present myself as cheerful and energetic, as though I haven’t got terminal cancer. Even writing that, to you as an unknown and voluntary reader, I felt a quiver of something, a wish to spare you, to not impose anything on you.
Tomorrow I am going on holiday to the west of the country with my son, who lives abroad. I have a tiny house there that I lived in forty years ago, briefly, and never sold. I feel nervous about the journey wearing me out, that the house will be in a bad state. Covid and illness have meant I haven’t been there since 2019. I know my son will look after me, and my partner has told him particulars about what to do if I feel unwell, ( which is go to A and E and get help), and how to prevent me overdoing it, as much as that is possible.
I know I’m likely to have a very nice time, as I usually do, and being away from everything here will be good for me.
Copyright Tuppence King
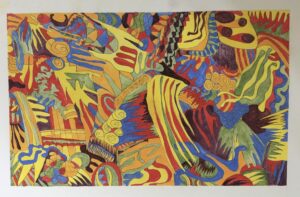
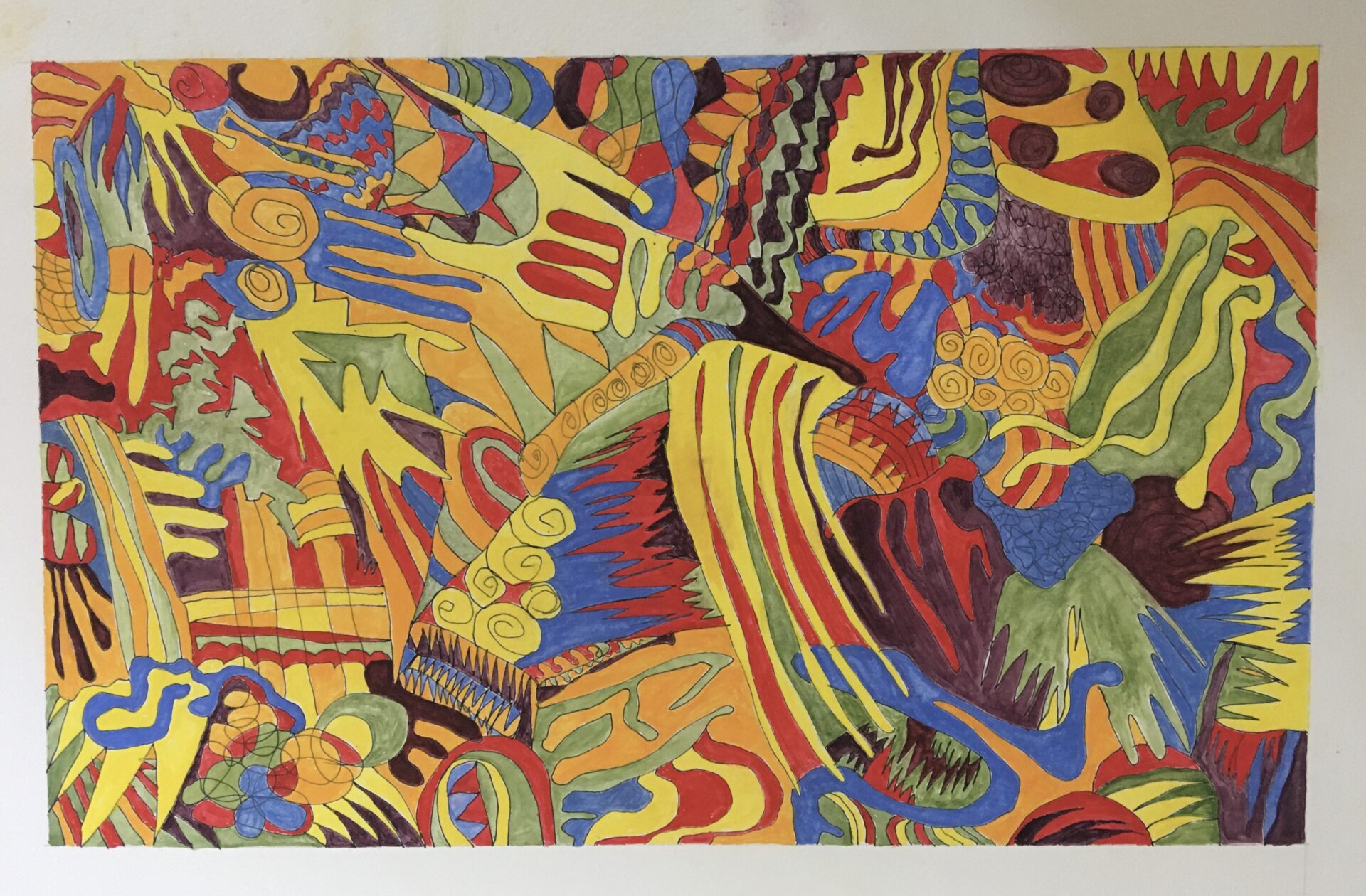
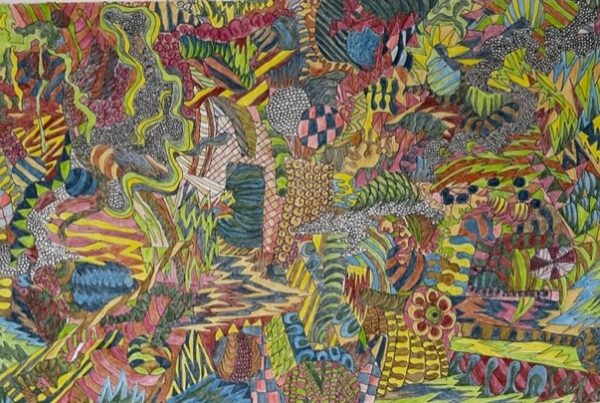
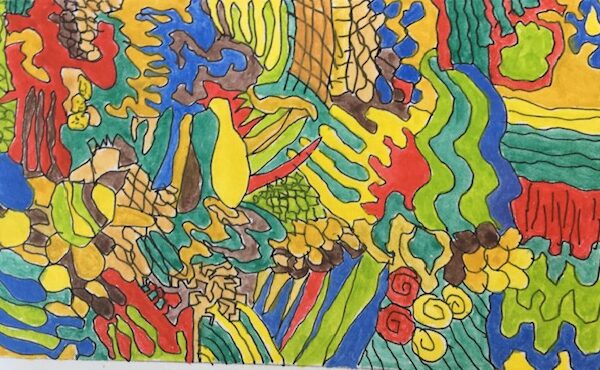
Painting by Tuppence King ©